Tartaczna 2
Discover the quality of healthcare in the style of Tartaczna2!


In each trimester of pregnancy, mothers-to-be should undergo a specific set of recommended examinations. One of the basic examinations in the third trimester is CTG, or cardiotocography.
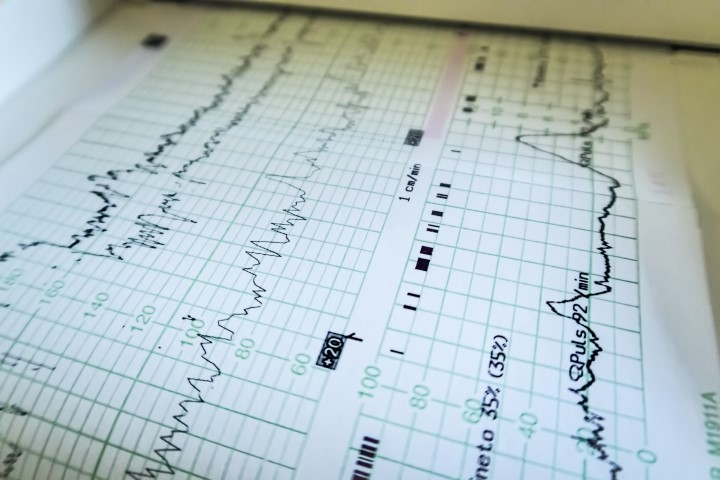
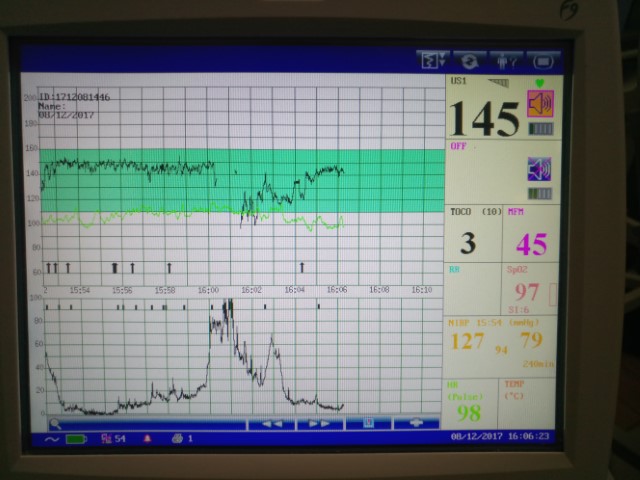
Cardiotocograph simultaneously records foetal heart rate and uterine contractions. A physician can combine both parameters in order to assess well-being of the baby at the very end of pregnancy or during labour.
CTG consists of two tests: tocometry and cardiography. Cardiography is continuous recording of the foetal heart rate, using an electrocardiograph or ultrasonic probe. We assess the systolic and diastolic cardiac function and fluctuations in frequency over small periods of time. Tocometry, in turn, records uterine contractions, using an external sensor.
There two types of CTG: a so-called nonstress test (NST) and an oxytocin challenge test (OCT). A nonstress test is a conventional CTG, measuring frequency and variability of the heart rate, which we can correlate with movements of the foetus. During an oxytocin challenge test, on the other hand, a woman receives small doses of oxytocin, the hormone responsible for uterine contractions.
An oxytocin challenge test is usually performed in the delivery room after the expected date of delivery or when recording of a nonstress CTG is inconclusive and diagnostics must be extended.
During CTG, 2 sensors (transducers) are placed against the mother's abdomen and are connected to a monitor. One is placed near the pelvic floor and the other in the place where the baby's heartbeat can be best heard. The whole recording is analysed by a computer and finally evaluated by a gynaecologist. During the test, a woman should not change her body position, and should preferably lie on her left side to avoid vena cava compression.

Duration of CTG recording is usually 20 to 30 minutes.
If the result is inconclusive or negative, the monitoring may be extended to about an hour. It is not necessarily an indication of abnormality. It may happen when the baby sleeps, and thanks to the extension a physician can into account the time the foetus is asleep during the monitoring.
We need to distinguish two dates: CTG at the end of pregnancy and during labour. Obviously, CTG is most useful in the perinatal period. It may also be performed earlier, even from the 24th week of pregnancy, if there are indications to it. However, sensitivity of such tests is vitiated by a high false-positive rate due to still immature foetal heart.
Perinatal ECGs are most accurate after 30-34 weeks of pregnancy.
While CTG during labour can provide a lot of important information, including whether a woman can have a natural birth or whether a caesarean section will be necessary.
CTG on the day of planned labour or during labour is recommended to every pregnant woman. Earlier CTG monitoring is recommended in the case of high-risk pregnancies and problems experienced by a mother-to-be during pregnancy. If there is a risk of foetal hypoxia or even intrauterine death.
The main indications include:
CTG monitors foetal well-being, i.e. a heart rate, heart rate deceleration and acceleration as well as duration of the acceleration phases. We can relate this data to foetal movement. Depending on CTG results, we determine whether the foetus is well oxygenated and whether placental hypoxia has not occurred.
Normal ranges for foetal heart rate are between 110 and 160 beats per minute, i.e. about twice as fast as a heart rate of an adult person. A heart rate greater than 160 beats per minute in at least 10-minute epochs is known as tachycardia. It may indicate an infection. If the heart rate is lower than 110 beats per minute in at least 10-minute epochs is known as bradycardia, which is usually caused by foetal hypoxia.
CTG also detects so-called oscillations, or slight fluctuations of the foetal heart rate. A correct acceleration result should range from 5 to 25 beats per minute. Accelerations can be caused by many factors, including foetal movement. FHR variability of less than 5 beats per minute may be related to foetal sleep, while no variability may indicate hypoxia.
A physician carefully correlates and analyses all the data obtained during the monitoring in order to give an accurate diagnosis.
A nonstress test (NST) is a non-invasive examination with no contraindications. The exceptions include a few pregnancy pathologies, such as placental abruption. In such cases, a physician decides on further action.
CTG does not require any special preparation. However, in order to obtain the most reliable and accurate result, a mother-to-be should eat a meal about 1-2 hours before the test. If a woman comes to the examination hungry, the foetus may show unnatural symptoms, wheezing or agitation.
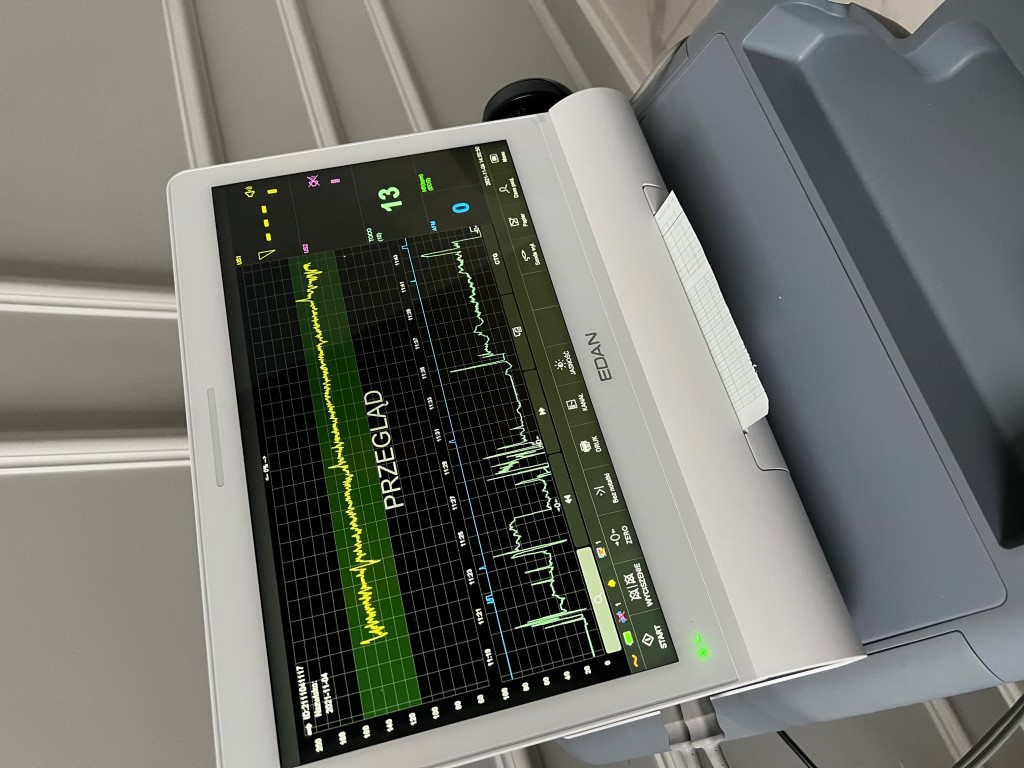
Tartaczna 2 Medical Centre has the highest quality CTG device: EDAN F15 cardiotocograph. The latest monitoring technology with automatic computer analysis currently available on the market.
Make an appointment with a midwife – online, by email (kontakt@tartaczna2.pl) or by phone: 58 719 10 25. The test can also be performed during an appointment with our gynaecologist after telephone confirmation.